Case Study
Posted on

Therapeutics derived from human plasma are vital for individuals with specific deficiencies but come with significant challenges. Plasma-derived products are expensive to produce, carry the potential risk of transmitting blood-borne diseases from donors to patients, and are subject to supply shortages and donor variability. To address these issues, tightly regulated manufacturers have begun producing synthetic alternatives.
A/Prof Ruby Law, Professor James Whisstock and their team in the Department of Biochemistry and Molecular Biology at Monash University are working to develop a synthetic alternative to plasminogen, which is a critical plasma-derived product essential for wound healing and the breakdown of blood clots.
‘There is a global supply shortage of plasminogen. Furthermore, therapeutic native plasminogen is short-lived, requiring patients to undergo frequent hospital infusions,’ A/Prof Law says.
‘The development of synthetic plasminogen could revolutionise treatments for wound healing, including diabetic wounds, pressure injuries (bedsores) and burn lesions.’
With the support of an Australia’s Economic Accelerator Seed grant and industry partner BioCurate, the team have successfully designed and identified lead synthetic plasminogen candidates to create more stable and accessible supplies.
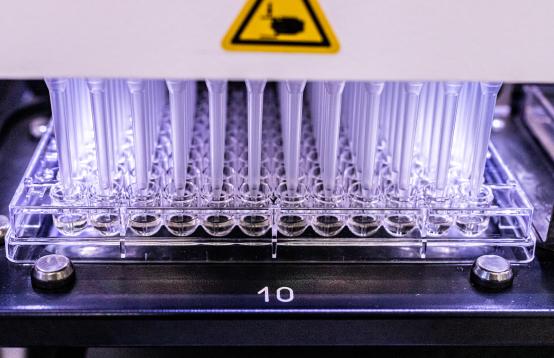
Collaborating with certified manufacturers, they demonstrated that these fully functional designer proteins can be produced commercially.
With interest from several international pharmaceutical companies and clinical collaborators, the team is exploring its potential applications in a variety of human diseases.
In preclinical studies with the Australian Regenerative Medicine Institute, they confirmed that synthetic plasminogen is highly functional in disease models, showing the potential to outperform plasma-derived products.
The team is now working with partners at the Australian Centre for Blood Diseases and Vanderbilt University, Tennessee to further compare the safety and efficacy of these designer proteins with plasma-derived products.
‘This partnership is critical to making this valuable biologic accessible to patients who depend on plasminogen for survival due to genetic deficiencies or as a clinical adjunct for wound healing,’ A/Prof Law says.
Professor Whisstock says the support of AEA and industry partner BioCurate is essential in making plasminogen available in Australia and globally. ‘This project restores hope for patients who have been deprived of a normal life,’ he says.
BioCurate, a joint initiative of the University of Melbourne and Monash University supported by the Victorian State Government, focuses on translating promising biomedical research into pre-clinical candidates for novel human therapeutics.
Kathy Nielsen, CEO of BioCurate, said: ‘As an Industry Partner, BioCurate is proud to support A/Prof Ruby Law, Prof James Whisstock and their team with our Proof-of-Concept Funding, to accelerate the translation of next generation therapies for treating chronic wounds and plasminogen deficiency’.
This project represents a significant step toward developing synthetic plasminogen for widespread clinical use. By addressing the limitations of plasma-derived products, synthetic plasminogen has the potential to deliver a safer, more reliable, and cost-effective therapeutic option for patients worldwide.
AEA is a $1.6 billion Australian Government investment aimed at transforming Australia’s research translation and commercialisation landscape.
Read more about the AEA program and follow the AEA LinkedIn page for regular updates.